Medicare Supplement Plans: Your MediGap Guide for 2026
Medicare Supplement Plans Guide
By Lou Spatafore – Updated Mar 10, 2025
Reviewed by Leslie Jablonski
Fact checked by Mike Montes

Take Advantage of Our Free Instant Quote System to Compare Medicare Supplement Plans
Since its inception in 1965, Medicare has been a vital safety net for millions of American senior citizens.
But it doesn’t cover everything. Not by a long shot. And it is not designed to stand on its own. There are significant gaps in Medicare coverage. Even with Medicare, seniors are still potentially exposed to the risk of thousands of dollars in out-of-pocket health care costs.
A recent study from Fidelity Investments found that the average retired couple age 65 may need approximately $315,000 saved (after tax) to cover health care expenses in retirement.
And that’s where Medicare supplement insurance, or “MediGap” comes in: MediGap insurance exists to help Medicare beneficiaries fill in the “gaps” in Medicare coverage: In exchange for a small, affordable, and predictable monthly premium, MediGap plans shield members from large and unexpected or unpredictable out-of-pocket costs for Medicare-approved services.
Medicare Basics
To understand how MediGap works, you should understand the basic parts and structure of Medicare, including what each part covers – and what it doesn’t.
Original Medicare (Parts A and B)
The term “Original Medicare” refers to the two main “parts” of Medicare that came into being with the passage of Title XVIII of the Social Security Act of 1965. Seniors are normally automatically enrolled in Medicare Part A and B when they first become eligible at age 65.

Medicare Part A is Hospital insurance. Medicare Part A covers most hospitalization charges for Medicare beneficiaries. It covers inpatient hospital stays, skilled nursing facilities, hospice care, home health care, and certain non-custodial nursing home care.

Medicare Part B is Medical Services insurance. This optional plan covers physicians’ charges, lab fees, blood, and durable medical equipment like oxygen machines, electric wheelchairs. Some people put off enrolling in Part B because they still receive benefits from a health plan at work.
If you fail to enroll in Part B during your Medicare Initial Enrollment Period (normally a 7-month period surrounding the month in which you turn age 65), and you did not maintain credible coverage in the interim, you may have to pay a lifetime penalty of 10% of the normal Part B premium.
Newer Medicare Programs

Medicare Part C (Medicare Advantage) provides Medicare beneficiaries with an optional way to use a private managed care organization to access their benefits under Medicare Parts A and B.
Some Medicare Advantage plans include prescription drug coverage. Others don’t, but you can purchase a separate, standalone prescription drug plan. Others don’t.
Medicare Advantage serves a similar function to MediGap: Fill in the gaps in coverage and potential out-of-pocket costs for MediGap. However, they are structured very differently.
You should not enroll in Medicare Advantage and MediGap at the same time.

Medicare Part D covers prescription drug charges for Medicare beneficiaries, subject to certain deductibles, coinsurance, and co–pays. These plans are optional. You will not be automatically enrolled in Medicare Part D. You must opt in.
These are the basic segments of Medicare.
Each of them serves an important purpose. But Original Medicare, especially, still leaves seniors exposed to significant expenses in the form of deductibles, co-insurance, co-pays, and limitations on covered hospital stays.
Medicare Part A. As of 2025, Medicare Part A kicks in only after you have covered the $1,676 deductible ($1,632 for 2024).
In addition, even with Medicare Part A, you will be responsible for paying co-pays for hospital stays as follows (as of 2026).
- Days 1-60: $0 (after you pay your Part A deductible)
- Days 61-90: $419 in 2025.
- Days 91-150: $838 copayment each day while using your 60 lifetime reserve days (as of 2025).
- After day 150: You pay all costs.
It’s easy to see how fast your out-of-pocket costs can add up if you have one or two significant hospitalizations or more, or long stays in covered nursing facilities.
And those costs are just the beginning.
Medicare Part B only covers 80% of costs. You are responsible for covering the remaining 20%. With high-cost durable medical equipment and physicians’ fees for expensive or repeated procedures, you may face thousands in additional out-of-pocket costs – unless you take action by covering them under a Medicare supplement plan or Medicare Advantage plan.
There is also a Medicare Part B deductible of $257 as of 2025.
Medicare supplement insurance is an affordable, realistic, and flexible way for seniors to plug those gaps in coverage, smooth out their Medicare spending, and blunt the financial effects of significant and costly medical events, such as hospitalizations and chronic disease treatment.
TIP: The best time, by far, to buy a MediGap policy is during your initial MediGap Enrollment Period, beginning the first day of the month in which you are both age 65 or older and enrolled in Medicare Part B.
See the “When To Buy MediGap” section below.
Compare Medicare Supplement Plans and the Carriers We Offer

























About Medicare Supplement Plans
Medicare supplement plans are sold by private insurance companies – many of which are household names among American consumers. Examples include Blue Cross/Blue Shield, Mutual of Omaha, Humana, UnitedHealthCare, Aetna, and many others.
These insurance companies are regulated by the Department of Medicare and Medicaid Services, as well as by state insurance commissioners.

MediGap is the secondary insurer, with Medicare as the primary. If you have a MediGap policy, Medicare will pay its share of the Medicare‐approved amounts under Original Medicare (Parts A and B) for covered health care costs.
Medicare doesn’t pay any of the costs of buying a MediGap policy. You are responsible for purchasing and paying for MediGap premiums out of your own pocket.
There isn’t one. MediGap and Medicare supplement plans are the same thing. The terms here are used interchangeably.
Note that Medicare Advantage is a very different program than Medicare supplement insurance/MediGap.
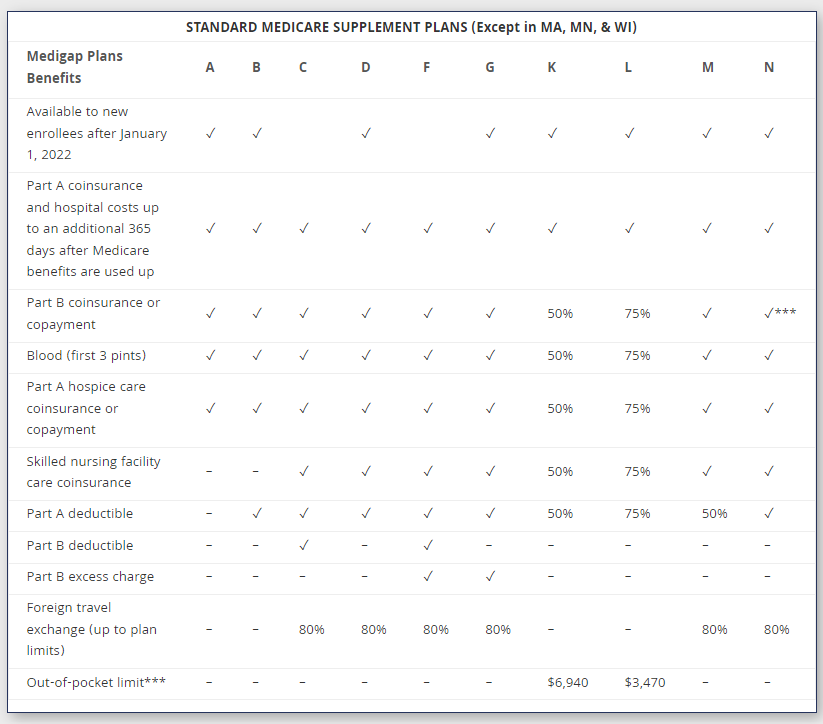
As of 2022, there are ten standard MediGap insurance plans, each authorized by the U.S. Department of Medicare and Medicaid Services. These plans, designated A through N, are standardized across the United States, except in three states that have adopted different standard plans. These three states are Massachusetts, Minnesota, and Wisconsin.
Because the plans are standardized, each plan under a given letter name must offer the same basic set of benefits and exclusions, no matter what company you buy it from.
The price (monthly premium) differs from company to company. But the basic set of benefits won’t: A Medicare Supplement Plan G from Humana will have the same basic benefits as a Medicare Supplement Plan G from Blue Cross/Blue Shield, or from any other carrier in the market.
So it’s pretty easy to compare plans from different insurance companies.
Each of these Medicare supplement plans provides a different mix of benefits. However, all of them will cover your Part A coinsurance costs and hospital costs for up to 365 days after you use up your benefits under Original Medicare.
Furthermore, they all cover all or part of your 20% share of expenses under Medicare Part B for lab fees, doctors’ fees, durable medical equipment, and outpatient expenses.
All MediGap plans except for Plan K and Plan Lalso cover all costs for hospice care. Plan K covers 50% of hospice costs, and Plan L covers 75% of costs.
All plans cover 100% of out-of-pocket hospice care costs, except for Plan K and Plan L, which cover 50% and 75% of hospice costs, respectively.
Most plans cover up to 80 percent of costs for care provided outside of the United States, which makes Medicare Advantage.
Generally not. Standard MediGap plans allow you to use your benefits with any provider that accepts Medicare patients, anywhere in the country.
This is one important way that MediGap differs from Medicare Advantage plans: Medicare Advantage relies on managed care organizations such as HMOs that save costs by negotiating discounted prices from care providers in a given area in exchange for a steady flow of patients. Outside of the network area, patients may have very limited options.
They then require patients to get non-emergency care from providers within the network, or they sharply restrict what they will pay.
It’s one of the great tradeoffs in the medical industry: The narrower the network, the greater the discounts the HMO can negotiate, all things being equal. So that lowers costs. But narrow networks also reduce choices available to patients.
However some Medicare Advantage plans allow patients access to their Medicare benefits at greatly reduced premiums. There’s even a zero-premium option available in many areas.
MediGap Advantages
MediGap plans have a number of advantages in common, compared to Medicare Advantage plans:
Freedom to choose your own provider – anywhere in the United States.
No referral required to see a specialist. HMOs and other managed care plans control costs by requiring patients to get a referral from their primary care doctor before they can see a specialist.
This is routine in Medicare Advantage. But MediGap plan members can go directly to any specialist who takes Medicare patients.
Foreign travel benefits. Medicare supplement plans C, D, F, G, M, and N include foreign travel benefits. These plans may be a good choice for people who plan to travel outside the United States in retirement.
 What are the most popular Medicare supplement plans?
What are the most popular Medicare supplement plans?
As of 2021, the most popular MediGap plan is also the most comprehensive: Plan F, according to research from America’s Health Insurance Plans (AHIP.org).
But Plan F is closed to new Medicare benficiaires.
The second most popular plan, with 22% of all MediGap beneficiaries enrolled, is Plan G
Plan N is the third most popular plan, at 10% of all MediGap beneficiaries enrolled. It’s also the 2nd most comprehensive plan available to new Medicare employees.
The fourth most popular is Plan C, which is also among the most comprehensive plans in MediGap. But like Plan F, Plan C is closed to new Medicare beneficiaries.
 Save Money With a High-Deductible MediGap Plan
Save Money With a High-Deductible MediGap Plan
If you have some savings, and you’re able to absorb some more of your health care costs, and you’re in decent health, you might consider a high-deductible MediGap plan. These plans require you to pick up more of your medical costs. But premiums are generally much lower.
Plan F and G both have high-deductible versions available in some areas. The Plan F version is not available to those who weren’t already Medicare-eligible as of January 1st. 2020. But new enrollees can still buy a high-deductible Plan G.
If you get a high‐deductible MediGap plan, you must pay for Medicare‐ covered costs (coinsurance, copayments, and deductibles) up to $2,870 (as of 2025) before your policy will pay anything.
You must also pay a separate deductible ($250 per year) for foreign travel emergency services.
STANDARD MEDICARE SUPPLEMENT PLANS (Except in MA, MN, & WI)
| MediGap Plans Benefits | A | B | C | D | F | G | K | L | M | N |
|---|---|---|---|---|---|---|---|---|---|---|
| Available to new enrollees after January 1, 2022 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Part A coinsurance and hospital costs up to an additional 365 days after Medicare benefits are used up | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Part B coinsurance or copayment | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 50% | 75% | ✓ | ✓*** |
| Blood (first 3 pints) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 50% | 75% | ✓ | ✓ |
| Part A hospice care coinsurance or copayment | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 50% | 75% | ✓ | ✓ |
| Skilled nursing facility care coinsurance | – | – | ✓ | ✓ | ✓ | ✓ | 50% | 75% | ✓ | ✓ |
| Part A deductible | – | ✓ | ✓ | ✓ | ✓ | ✓ | 50% | 75% | 50% | ✓ |
| Part B deductible | – | – | ✓ | – | ✓ | – | – | – | – | – |
| Part B excess charge | – | – | – | – | ✓ | ✓ | – | – | – | – |
| Foreign travel exchange (up to plan limits) | – | – | 80% | 80% | 80% | 80% | – | – | 80% | 80% |
| Out-of-pocket limit*** | – | – | – | – | – | – | $7,220 | $3,610 | – | – |
Medicare SELECT: A Lower-Cost Alternative
In some states, you may be able to buy a special type of MediGap policy called Medicare SELECT. Medicare SELECT plans are hybrids: They may require you to see certain providers for non-emergency care, but also may cost less per month than other MediGap plans.
If you’re on a budget, and you’re not worried about not being able to choose your own doctor, then electing a Medicare SELECT MediGap plan or a zero-premium Medicare Advantage plan may be good options for you, depending on what’s available in your area.
Standard Medicare Supplement Plans
You can view all the standard MediGap plans as adopted in 47 states plus the District of Columbia here.
Medicare SELECT: A Lower-Cost Alternative
In some states, you may be able to buy a special type of MediGap policy called Medicare SELECT. Medicare SELECT plans are hybrids: They may require you to see certain providers for non-emergency care, but also may cost less per month than other MediGap plans.
If you’re on a budget, and you’re not worried about not being able to choose your own doctor, then electing a Medicare SELECT MediGap plan or a zero-premium Medicare Advantage plan may be good options for you, depending on what’s available in your area.
Standard Medicare Supplement Plans
You can view all the standard MediGap plans as adopted in 47 states plus the District of Columbia here.
Can I Buy MediGap Plan F, Plan C, Plan E, Plan H, Plan I or Plan J?
Plans E, H, I, and J are no longer sold, but current Medicare beneficiaries who are already enrolled in one of those plans are usually grandfathered in.
Plan F and Plan C are also closed to new Medicare beneficiaries. But you can still buy them if you were eligible for Medicaid on or before January 1st, 2020.
These plans were hugely popular because they essentially covered all out-of-pocket expenses associated with Medicare. However, Congress eventually decided that they were too good a deal, and that people needed to participate in the cost in some way. So they closed those plans for people who were not already Medicare eligible.
If you aren’t eligible for Plan F or Plan C, the next most comprehensive plans are Plans G and N. Medicare Supplement Plan G covers all out-of-pocket costs for Medicare services under Part A and B, except for the Part B deductible of $257, as of 2025. Medicare Supplement Plan N covers everything except the Part B deductible and any physicians’ “excess charges” over and above the Medicare-approved rates, if your state allows excess charges.
Plan N also requires a copayment of up to $20 for some office visits, and up to a $50 copayment for emergency room visits that don’t result in a hospital admission.
If your state does not allow excess charges, then Plan N may be a slightly better deal than Plan G. But if you’re a frequent customer at your local Emergency Department, your co-pays might offset any premium savings from using Plan N rather than Plan G.
Give us a call and we’ll help you assess which of these plans might be the best one for your particular circumstances.
When to Buy MediGap
Your MediGap initial enrollment period is a limited six-month window that begins on the first day of the first month in which you are both age 65 or older and enrolled in Medicare Part B.
This time is the only time during your lifetime you enjoy a guaranteed enrollment privilege with MediGap plans. You have the right to buy any MediGap plan issued in your state, regardless of your medical history or condition.
They have to sell them at the best rate. As long as you buy during your initial enrollment period, the MediGap insurance company cannot charge you any more than they charge another person your age and sex and location with no medical issues. They can charge more for smokers, however.
If you’re overweight, have diabetes, heart disease, or a history of any kind of medical condition, you should definitely keep an eye on your initial enrollment period.
You can put off your initial enrollment period by delaying enrollment in Part B. This is common for people who still get medical insurance from an employer. But once your initial enrollment period ends and you haven’t already enrolled in MediGap, you will have to go through medical underwriting in the future.
That means that insurance companies can charge a higher premium due to your medical history, or even turn you down outright.
Some companies have stricter underwriting standards than others. Other companies are more willing to enroll people with diabetes, high blood pressure, or other conditions. But premiums for these plans are normally higher.
By buying a MediGap plan during your initial enrollment period, while you are still in good health, and before any new medical conditions can onset, you preserve your choices and you get access to the best risk pools.
Putting off the decision means paying higher MediGap premiums in the future, for life, loss of access to the more selective (and therefore lower-cost) MediGap carriers, and potentially being turned down outright for MediGap insurance.
A handful of states have adopted rules allowing Medicare beneficiaries an additional MediGap open enrollment period around their birthdays. During this window, they can enroll in MediGap without having to answer any questions about their health.
As of October 2022, these states are California, Oregon, Idaho, Illinois, Louisiana, and Nevada.
Specific rules, deadlines, criteria differ in each of these states.
Medicare itself will cover your pre-existing conditions. But the MediGap plan may not pay its part for that period. So may have to pay deductibles, co-insurance, and copays related to the treatment of your pre-existing condition for up to six months after you enroll in a MediGap plan.
This is called the “pre-existing condition waiting period.”
However, this is only temporary.
After six months, the MediGap plan will begin to pay benefits for treatment of that particular condition.
Again, though, buying MediGap insurance when you’re first eligible, during your initial enrollment period, means you won’t have to worry about any waiting periods. Your MediGap policy will pay benefits for treatment of your pre-existing condition from the first day.
In some circumstances, switching MediGap plans when you are first eligible
MediGap Prices
Because MediGap is sold by private insurance companies, they are generally free to set their own pricing. Different MediGap plans therefore have different prices.
MediGap companies have three broad approaches to pricing, each has advantages and disadvantages.
- Medicare provided by a private
company - $257 deductible for Medicare
Part B, as of 2025. Plan G covers
all other out of pocket costs for
Part A and B services. - Can see any provider
- See specialist without referral
- Good anywhere in the U.S.
- Some plans provide 80%
coverage for care outside the
U.S. - Varies, but can be up to
$400+/month for a Plan G - No prescription drug coverage
- You pay premiums, plus $257
Part B deductible - Depends on plan. But Plans F
and G have no copays - Guaranteed issue within 6
months of enrolling in Medicare
Part B - Mayo/Cleveland Clinic included
- Community rating: Everyone in the plan pays the same price, regardless of age. That means younger members effectively subsidize older members – but benefit as they themselves get older, since prices don’t increase as much as they would in an attained age-rated system.
- Issue age-rated: The company sets premiums based on your age when you first enroll in the plan. People who enroll when first eligible therefore enjoy lower premiums than people who delay enrollment.
- Attained age-rated: Premiums are based on your age now. So premiums are low when you first enroll, and then steadily increase as you get older.
Comparing MediGap and Medicare Advantage
- Traditional insurance plan
- Plans Vary
- Non-emergency care must
stay within network - Must get a referral from PCP
with HMOs but not PPOs - Most networks are regional
- Must stay within the U.S.
- Varies, but many zero-premium plans available
- Some plans include
prescription drug coverage - Premiums (sometimes),
deductibles, co-pays,
coinsurance - Copays are typical
- Guaranteed issue during initial
eligibility period and annual
election period
(limited window to enroll) - High-tier providers may not
included in network
|
|
|
|---|---|
| Private insurance companies | |
| Cover all Medicare Part A and Part B benefits | |
| No prescription drug coverage (consider buying a Part D plan) | |
| Foreign travel benefit in some plans | |
| No care network restrictions (exception: Medicare SELECT) | |
| Can be used anywhere in the country | |
| Any doctor who takes Medicare patients | |
| Always have premiums | |
| No specific special needs programs | |
| No ‘non-medical’ benefits. | |
| Generally not suitable for Medicaid beneficiaries |
|
|
|---|
| Private insurance companies |
| Cover all Medicare Part A and Part B benefits |
| Some plans include prescription drug coverage. Some plans don’t. |
| Normally no foreign travel benefit |
| You must normally get non-emergency treatment within your care network |
| Usually limited coverage outside of geographic area |
| Restricted care networks |
| Zero-premium options available in most areas |
| Special needs programs |
| More non-medical benefits in some plans (e.g., transportation services, meal delivery, grocery delivery, home modification benefits, etc., in some areas |
| Special programs for “dual eligible” patients simultaneously enrolled in Medicare and Medicaid. |
Medicare Supplement Plans and Prescription Drugs
Note: If you want some expert assistance in deciding which of these strategies is the best fit for you, we’re happy to help! Just click here to make an appointment for a free consultation with a MediGap Advisors Personal Benefits Manager.
Or if you are ready, click here sign up to enroll in Medi-Share 65+ right away! It’s easy, and takes just minutes.
Medicare Supplement Plans vs. Health Sharing
Health sharing is a less well-known, but increasingly popular non-insurance alternative that can help shield you from high unexpected medical costs – often at just a fraction of the cost of traditional insurance-based approaches.
One of these innovative healthsharing plans, the Medi-Share 65+ plan, is designed specifically for Medicare beneficiaries.
How Medi-Share Healthsharing Works
Medi-Share is not an insurance company. Instead, Medi-Share is a non-profit health sharing ministry organization where more than 400,000 members agree to live healthy, responsible lifestyles in accordance with Biblical values, and who agree to share each other’s medical bills.
Each Medi-Share 65+ member makes a monthly contribution to the plan to help share fellow members’ expenses. Medi-Share simply facilitates the collection, need verification, and distribution of member contributions to those in need.
Click here to learn more about the health sharing concept, in general.
Medi-Share 65+ Sharing Benefits
Like MediGap plans, Medi-Share 65+ helps Medicare beneficiaries enrolled in the plan pay out-of-pocket costs for services approved under Original Medicare but that Medicare doesn’t pay, specifically, Part A and B deductibles, co-pays, and coinsurance.
Under Medi-Share 65+, plan members are responsible for the first $500 in Original Medicare charges per family (not per individual).
After that, 100% of your costs for services approved under Original Medicare are 100% shareable. That is, you don’t pay them out of pocket. Your fellow Medi-Share members pick up the cost. You just continue to make your monthly sharing contribution, which helps others in need.
Medi-Share’s 65+ sharing benefits are similar to those of MediGap Plans G and N. But Medi-Share 65+ is available for a significantly lower monthly outlay.
No Provider Network Restrictions
Like MediGap plans (and unlike Medicare Advantage), Medi-Share 65+ allows you to use your sharing benefits with any doctor or provider. You can choose your own doctor, and you are not limited to any specific care network for non-emergency care.
Pricing
While MediGap Plan G plan pricing runs from $160 and up in most areas, Medi-Share 65+ plans start at just $99 per month for those aged 65 to 74, and just $150 per month for those aged 75 and older.
Pricing is the same regardless of your location.
Furthermore, Medi-Share 65+ also comes with a price lock-in guarantee: If you sign up before you turn 75, Medi-Share will lock in your pricing until your 75th birthday. That’s up to a ten-year price guarantee, if you sign up at age 65!
Sign up for Medi-Share 65+ in minutes!
Your Private Medicare Strategy Options at a Glance
This table illustrates the basic features, benefits, and limitations of each of your private Medicare strategy options.
Medi-Share 65+ healthsharing, MediGap, and Medicare Advantage each have important advantages and disadvantages. There is no “one-size-fits-all” option. The best plan for you depends on your medical status, location, budget, and many other factors.
Medi-Share 65+
- Non-insurance alternative
- Shares All Deductibles, Co-pays,
and Co-insurance for Medicare
Parts A and B over $500
member
responsibility amount - Can see any provider
- See specialist without referral
- Good anywhere in the U.S.
- Can use outside of U.S.
- Low monthly contributions ($99
for ages 65-74, $150 for ages
75+, anywhere in the U.S. - No prescription drug coverage
- You pay monthly sharing
amount, + member
responsibility amount - No copays to providers
- Medical underwriting required
to join - Mayo/Cleveland Clinic included
MediGap Plan G
- Medicare provided by a private
company - $226 deductible for Medicare
Part B, as of 2023. Plan G covers
all other out of pocket costs for
Part A and B services. - Can see any provider
- See specialist without referral
- Good anywhere in the U.S.
- Some plans provide 80%
coverage for care outside the
U.S. - Varies, but can be up to
$400+/month for a Plan G - No prescription drug coverage
- You pay premiums, plus $226
Part B deductible - Depends on plan. But Plans F
and G have no copays - Guaranteed issue within 6
months of enrolling in Medicare
Part B - Mayo/Cleveland Clinic included
Medicare Advantage
- Traditional insurance plan
- Plans Vary
- Non-emergency care must
stay within network - Must get a referral from PCP
with HMOs but not PPOs - Most networks are regional
- Must stay within the U.S.
- Varies, but many zero-premium plans available
- Some plans include
prescription drug coverage - Premiums (sometimes),
deductibles, co-pays,
coinsurance - Copays are typical
- Guaranteed issue during initial
eligibility period and annual
election period
(limited window to enroll) - High-tier providers may not
included in network
Your Private Medicare Strategy Options at a Glance
This table illustrates the basic features, benefits, and limitations of each of your private Medicare strategy options.
Medi-Share 65+ healthsharing, MediGap, and Medicare Advantage each have important advantages and disadvantages. There is no “one-size-fits-all” option. The best plan for you depends on your medical status, location, budget, and many other factors.
| Medi-Share 65+ | Medigap Plan G | Medicare Advantage |
|---|---|---|
| Non-insurance alternative | Medicare provided by a private company | Traditional insurance plan |
| Shares All Deductibles, Co-pays, and Co-insurance for Medicare Parts A and B over $500 member responsibility amount | $257 deductible for Medicare Part B, as of 2025. Plan G covers all other out of pocket costs for Part A and B services. | Plans Vary |
| Can see any provider | Can see any provider | Non-emergency care must stay within network |
| See specialist without referral | See specialist without referral | Must get a referral from PCP with HMOs but not PPOs |
| Good anywhere in the U.S. | Good anywhere in the U.S. | Most networks are regional |
| Can use outside of U.S. | Some plans provide 80% coverage for care outside the U.S. | Must stay within the U.S. |
| Low monthly contributions ($99 for ages 65-74, $150 for ages 75+, anywhere in the U.S. | Varies, but can be up to $400+/month for a Plan G | Varies, but many zero-premium plans available |
| No prescription drug coverage | No prescription drug coverage | Some plans include prescription drug coverage |
| You pay monthly sharing amount, + member responsibility amount | You pay premiums, plus $257 Part B deductible | Premiums (sometimes), deductibles, co-pays, coinsurance |
| No copays to providers | Depends on plan. But Plans F and G have no copays | Copays are typical |
| Medical underwriting required to join | Guaranteed issue within 6 months of enrolling in Medicare Part B | Guaranteed issue during initial eligibility period and annual election period (limited window to enroll) |
| Mayo/Cleveland Clinic included | Mayo/Cleveland Clinic included | High-tier providers may not included in network |
Note: If you want some expert assistance in deciding which of these strategies is the best fit for you, we’re happy to help! Just click here to make an appointment for a free consultation with a Medigap Advisors Personal Benefits Manager.
Or if you are ready, click here sign up to enroll in Medi-Share 65+ right away! It’s easy, and takes just minutes.
Note: If you want some expert assistance in deciding which of these strategies is the best fit for you, we’re happy to help! Just click here to make an appointment for a free consultation with a MediGap Advisors Personal Benefits Manager.
Or if you are ready, click here sign up to enroll in Medi-Share 65+ right away! It’s easy, and takes just minutes.
Buying Medicare Supplement Plans
The vast majority of MediGap salespeople are honest. But there have been a few incidents of unethical sales practices around the country.
Here’s what to be aware of when you’re buying a Medicare supplement plan:

Can I Switch Medicare Supplement Plans?
Can I Switch Medicare Supplement Plans?
Sometimes people want to switch from one Medicare supplement plan to a different one.
There are several good reasons you might want to do this:
- You need new benefits you didn’t need before, such as foreign travel benefits, and you want to switch to a plan that has them.
- You’re overpaying for benefits you no longer need.
- You aren’t happy with your insurance company’s customer service, communication, or claims payments.
- You find the same plan available for a lower premium.
Switching MediGap Plans and Guaranteed Enrollment Rights
In most states, you only have a right to switch from one MediGap policy to another if:
A. you’re within your six-month MediGap Open Enrollment Period, or;
B. you’re eligible for guaranteed issue rights because of specific circumstances.
Outside of these circumstances, you don’t have an automatic right to be accepted by another MediGap plan provider. To switch outside of these circumstances, you must pass medical underwriting. That means you could be “rated up” (required to pay a higher premium due to your medical history) or turned down altogether.
MediGap plans aren’t subject to the same Affordable Care ACT rules that otherwise force insurance companies to accept applicants with pre-existing medical conditions. MediGap plans only have to take you during your initial enrollment period, or under specific life conditions (such as your existing plan being terminated).
Some states have less stringent rules on switching between MediGap plans than others.
Go here to read more about Medicare supplement plan open enrollment periods.
What to Consider When Switching Medicare Supplement Plans
If you’re in good health, you may well pass medical underwriting, and be able to find another MediGap provider who will accept you. Your premium may go up, however, due to you being older than you were when you first enrolled in MediGap.
Before switching, be sure to compare all aspects of both MediGap plans, including not only current premiums, but the outlook for future premium increases, before switching. For example, some MediGap plans will guarantee level premiums for life to customers who sign on during the open enrollment period.
Switching to a plan that has attained age pricing, and out of a plan with a guaranteed level premium lock-in may save money in the short run. In the long run, you may be exposed to significant premium increases in future years, as you get older.
Also, be aware that there are some benefits available in MediGap plans that were purchased prior to 2010 that aren’t available today.
What is the MediGap “Free Look” Period?
When you enroll in a new MediGap policy, you have up to 30 days by law from the time your new policy is delivered to look over your policy documents. Make sure the plan’s benefits and premiums match your understanding from the insurance agent who sold you the policy.
If you decide you don’t want the plan, you can cancel at any time during the “free look” period, and keep the original plan.
However, you’ll need to pay two premiums for that month.
If you decide to keep the new one, be sure to cancel the old one. But don’t cancel your old MediGap policy before your new one is in force.
Can I Switch from MediGap to Medicare Advantage?
It is possible to switch from a Medicare Advantage plan to a Medicare supplement/MediGap plan. However, you can’t do so whenever you like. You must wait until the Medicare Advantage Annual Election period, which runs from October 15th through December 7th each year in most states.
If you want to switch back to MediGap after dropping your plan and going with a Medicare Advantage plan, you can only do so in the first 12 months of signing up with Medicare Advantage, or if this isn’t the first time you’ve dropped MediGap for Medicare Advantage, if you have guaranteed issue rights.
Can I Switch from Medicare Advantage to MediGap?
Yes, but in most cases you’ll have to go through medical underwriting. That means you could be turned down.
However, there are certain exceptions: If you’re relocating out of your Medicare Advantage plan’s service area, for example, or your Medicare Advantage plan was discontinued, you may qualify for guaranteed issue rights when you apply for your new MediGap plan.
In this case, you’ll have a six-month window, your MediGap enrollment period, in which to make the switch.
MediGap Open Enrollment vs. Medicare Open Enrollment
It’s important not to confuse the various Medicare-related enrollment periods, election periods, and deadlines.
MediGap Open Enrollment is your once-in-a-lifetime enrollment window that opens for a six-month window when you are at least age 65 and you enroll in Medicare Part B.
Your Annual Election Period comes every year, from October 15h through December 7th. During the annual election period, you are allowed to make changes to your Medicare Advantage coverage and certain other Medicare-related coverages.
During the annual election period, you may make any of these changes to your Medicare coverage:
- Change to a Medicare Advantage plan from Original Medicare, Part A and Part B.
- Change from a Medicare Advantage plan to Original Medicare, Part A and Part B.
- Change from one Medicare Advantage plan to another (regardless of whether either plan offers drug coverage).
- Enroll in Part D prescription drug plan.
- Change from one Medicare prescription drug plan to another.
- Drop prescription drug coverage completely.
Note that “enroll in a MediGap plan” is conspicuously absent from these choices. You can apply to a MediGap plan, but you are generally not entitled to a guaranteed enrollment privilege, except in very specific circumstances.
How To Buy Medicare Supplement Plans
 There’s a lot of information out there. It can seem overwhelming at times.
There’s a lot of information out there. It can seem overwhelming at times.
But it doesn’t have to be.
At MediGap Advisors, we make it easy for Medicare beneficiaries and retirees to learn about all your health care options. And then to select the right plan or combination of plans to suit your particular plans and budget.
Our process is low-pressure and consultative. We’ll ask you a series of questions to define your needs and what aspects of a Medicare strategy are most important to you and your family.
Then we’ll walk you through your choices, making sure you understand the advantages, disadvantages, and costs of each of your options under consideration.
The process is very easy, and low stress.
For more information, or to learn more about your options, click here, and set an appointment with one of our experienced Personal Benefits Advisors. Or if you prefer, don’t hesitate to call us at 800-913-3416.
